Pilates is another great exercise for relieving back pain because it focuses on strengthening your core muscles, which include the back.
Pilates exercises are very smooth and controlled movements, so there is little danger of getting injured while exercising. It’s also a great way work on your strength and flexibility, both of which help to alleviate back pain. . One of the best benefits of Pilates is that it helps improve posture, a common cause of lower back pain.
The following Pilates exercises benefit the spine and are appropriate for beginners. Do each exercise slowly and smoothly, and repeat ten times if you can. The key to pilates is quality of exercise, not quantity; it is more important to do fewer exercises slowly and correctly than to do all ten repetitions quickly.
THE HUNDRED:
Start by lying on your back with your legs either stretched out or bent at the knees, whichever is most comfortable. Raise your head and, if you can, your legs off the floor a few inches. If this puts too much stress on your lower back, just raise your head and keep your feet on the floor with your knees bent. Try to keep your neck relaxed. Now extend your arms, and raise and lower them about two inches. While doing this, inhale for a count of five and exhale for a count of five.
Sit with legs extended in front of you and slightly more than hip width apart and feet flexed. Inhale and pretend that you are hovering over an imaginary beach ball by leaning your upper body forward, arms extended, while rounding your back and pulling in your abdomen. Exhale as you sit back up slowly one vertebra at a time.
The ROLLUP:
Begin by lying on your back, legs extended, and arms stretched above your head with your shoulders on the floor. Alternately, you may want to do this exercise with your feet on the floor, knees bent. Inhale
and lift your arms toward the ceiling. Exhale and roll your torso forward, as if you are doing a full body sit-up. You should ideally roll into a sitting position, but if you can’t, just bring your torso as far off the mat as you comfortably can before returning to your starting position.
 The SAW: Sit with your legs slightly wider than hip width, feet flexed. Your arms should be extended straight out to the side. Sit up very straight as if you are trying to touch the ceiling with the top of your head. Exhale; turn your body to the left, keeping your arms in line with your shoulders, and bend over as if your hand is going to saw off your little toe. Inhale, return slowly to your original position, and repeat on the other side.
The SAW: Sit with your legs slightly wider than hip width, feet flexed. Your arms should be extended straight out to the side. Sit up very straight as if you are trying to touch the ceiling with the top of your head. Exhale; turn your body to the left, keeping your arms in line with your shoulders, and bend over as if your hand is going to saw off your little toe. Inhale, return slowly to your original position, and repeat on the other side.
SPINE TWIST: Sit with your legs slightly more than hip width apart and your arms extended out to the sides. Inhale, tighten your abs, and sit up very straight as if you are trying to touch your head to the ceiling. Now exhale and turn to the right as far as you comfortably can. This exercise is to increase your back mobility only, so do not stretch your back muscles. Inhale and return to your starting position. Repeat on the left side.
 Leg Circle with fit band
Leg Circle with fit band
1. Start by lying on your back and placing a band around the foot that is pointed towards the ceiling.
2. Holding the other end of the band with your hands allow your leg to fall towards the side.
3. Once your leg reaches the side then bring it back up to the top and let your leg fall toward the other foot.
4. Bring your leg back up and finish by shifting the leg to the other side.
5. Return to the starting position and repeat.
Pilates Saw on Stability Ball
1. Sit on stability ball with your legs straight and your arms outstretched to the side.
2. Rotate and twist your trunk so that your right hand reaches and touches your left foot.
3. Return to t he starting position and repeat to the other side.
he starting position and repeat to the other side.
Prone Single Leg Kick
1. Lie face down on the floor and legs straight.
2. Slowly curl one leg up until your foot hits your hip.
3. Return to the starting position and repeat with the other side.
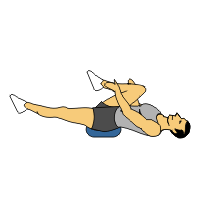
 Scissors
Scissors
1) Start position: Straighten both legs so that they are perpendicular to floor.
2) Slowly lower one leg to approximately 45°.
3) Return to start position and repeat.
4) Remember to maintain stability in lower back throughout movement by keeping abdominal muscles contracted - DO NOT ARCH LOWER BACK. To increase intensity, lower legs past 45° without touching floor as long as trunk stability is maintained